Management of Diabetic Ulcers Due to Arterial Insufficiency
Diabetes has emerged as one of the most significant health problems. About 10% of people are living with diabetes globally, including in the US. However, what is worrisome is that cases of diabetes continue to rise. Data shows that one-third of the US population is also living with prediabetes.
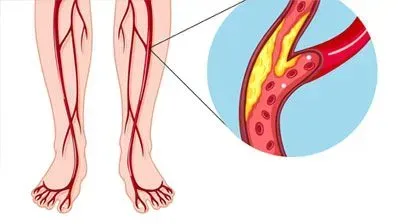
Diabetes causes numerous complications. It is especially bad for nerve and vascular health. Thus, diabetes causes complications like increased risk of cardiovascular diseases, peripheral vascular disorders, kidney disease, retinopathy, and diabetic ulcers.
Diabetic ulcers most commonly occur on the lower extremities (legs and feet). Poorly managed diabetic ulcers are the leading cause of amputations after trauma. If inadequately treated, ulcers penetrate the full skin thickness, get severely infected, and ultimately require amputation.
Understanding diabetic foot ulcers
Treating diabetic foot ulcers is quite complicated and requires a multidisciplinary team. It appears that there is a unique role of vascular surgeons and interventional radiologists in managing these ulcers and preventing amputations.
Studies show that there are two primary causes of foot ulcers in diabetes; purely neuropathic, purely ischemic (vascular issue), and mixed. It is estimated that just about 35% are purely neuropathic. Conversely, 65% of all ulcers are either purely ischemic/vascular or mixed.
Regretfully, for decades the role of peripheral arterial disease (PAD) was ignored in the diabetic foot. It may explain why the clinical outcomes were so bad. However, in recent years, the approach to the diabetic foot has changed. Most researchers now realize that PAD plays a significant role in the diabetic foot.
One of the most extensive studies to date, called The EURODIALE study, shows it is vital to differentiate diabetic ulcers based on the presence or absence of PAD. It is because those with PAD have a much lower healing rate. Moreover, such ulcers are at a greater risk of getting infected. But even worst, PAD ulcers are much more likely to end with food amputation.
How can doctors know if the diabetic ulcer is due to arterial insufficiency?
Thus, it is vital to differentiate between the neuropathic and PAD ulcers in diabetes. These are two quite different kinds of ulcers requiring different treatment approaches.
There are many ways of understanding arterial insufficiency. Some methods are non-invasive, and others are minimally invasive.
Color Doppler ultrasound (CDUS) is one of the excellent non-invasive says of visualizing the vascular blood flow. It provides a color map of blood flow through various blood vessels. It is one of the best methods in the way that it is safe, non-invasive, and doctors can check multiple arteries in a short time. However, it may be less sensitive in detecting minor arterial lesions, especially in smaller blood vessels.
Doctors may also use Multidetector-row computed tomography angiography (MD-CTA). It is minimally invasive and is a highly sensitive method. It is especially useful for small blood vessels of calves and other small blood vessels in the foot. In addition, it has a high resolution and is thus one of the most effective ways to diagnose the condition.
Contrast-enhanced magnetic resonance angiography (CE-MRA) is another highly useful and minimally invasive method.
Intra-arterial digital subtraction angiography is yet another way of diagnosing PAD. Doctors often do angiography in patients when they think that angioplasty or revascularization is needed. Thus, they may often carry out this procedure (or even other procedures) just before the intervention.
Thus, carrying out minimally invasive diagnostic procedures like angiography before revascularization has certain benefits. So, it is because doctors can use the same cut to introduce catheters for diagnostic reasons and treatment, thus improving the safety of the procedure and minimizing trauma.
Treatment of diabetic ulcer due to arterial insufficiency
Diabetic ulcers due to PAD must be treated with the help of either open surgery or endovascular revascularization. Needless to say, that less invasive methods like angioplasty are often preferred due to less trauma, faster healing, and much higher safety of the procedure.
Some individuals may ask if there is any need for revascularization in diabetic ulcers? Well, the studies show the clear advantage of revascularization. Comparative data from extensive studies show that revascularization may increase the healing rate by more than double. Not only that, revascularization may cut down the risk of amputation to half.
Since there is absolutely no doubt about the benefit of revascularization, the next question could be the choice of method. For most patients, the initial method of treatment could be balloon angioplasty. It is quite a safe procedure and is minimally invasive. Doctors use local anesthetics and introduce a catheter to blood vessels. Then, they use an x-ray monitor to visualize.
They use special instruments and catheters. These catheters have a balloon at their end. Once the catheter reaches the place where there is a plaque (as visible in the x-ray monitor), they inflate the balloon. This would reopen the artery, normalizing the blood flow.
However, quite often, dilation of the artery with a balloon is not enough. Thus, doctors would often put a metallic stent at the place. These stents support the artery wall, prevent their constriction. In addition, many stents are coated with medication to prevent the formation of plaques at that place in the future.
However, angioplasty and stents may not work in all. For example, some people are too prone to plaque formations. In such a case, doctors would need to carry out bypass surgery. As the name of the surgery suggests, it involves bypassing the occluded artery. For this, doctors would take some less needed artery from the patient’s body and use it to create a bridge that bypasses the plaque, thus restoring the blood flow.
To conclude, diabetic foot ulcer is a severe condition requiring a multidisciplinary team to treat the disease. It appears that interventional radiologists (those who carry out angioplasty or put stents in blood vessels) and vascular surgeons have a special place in improving healing rates and preventing foot amputation.
References
- National Diabetes Statistics Report, 2020 | CDC. Published September 28, 2020. Accessed December 24, 2021. https://www.cdc.gov/diabetes/data/statistics-report/index.html
- Brownrigg JRW, Apelqvist J, Bakker K, Schaper NC, Hinchliffe RJ. Evidence-based Management of PAD & the Diabetic Foot. European Journal of Vascular and Endovascular Surgery. 2013;45(6):673-681. doi:10.1016/j.ejvs.2013.02.014
- Armstrong DG, Cohen K, Courric S, Bharara M, Marston W. Diabetic Foot Ulcers and Vascular Insufficiency: Our Population Has Changed, but Our Methods Have Not. J Diabetes Sci Technol. 2011;5(6):1591-1595.
- Prompers L, Schaper N, Apelqvist J, et al. Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The EURODIALE Study. Diabetologia. 2008;51(5):747-755. doi:10.1007/s00125-008-0940-0
- Schaper NC, Andros G, Apelqvist J, et al. Diagnosis and treatment of peripheral arterial disease in diabetic patients with a foot ulcer. A progress report of the International Working Group on the Diabetic Foot. Diabetes/Metabolism Research and Reviews. 2012;28(S1):218-224. doi:10.1002/dmrr.2255