Diabetic Foot Infection – Veins And Vascular Clinic in Michigan
Metabolic disorders like obesity and diabetes are on the rise. For example, more than 11% of the population is living with diabetes in the US. It means that in some urban areas, even more than 15% of people may be living with diabetes, considering that diabetes prevalence is higher in urban centers.
Most of these are individuals living with type 2 diabetes, as the prevalence of type 2 diabetes is above 90% in the US. It is a chronic disorder, a diagnosis for a lifetime. It means that people living with diabetes struggle to control it adequately. As a result, most people living with diabetes have inadequate control over blood sugar levels.
Poorly controlled diabetes leads to a range of complications. Diabetes may cause both acute and chronic complications. However, the more significant concern is chronic complications of blood vessels and nerves when it comes to type 2 diabetes.
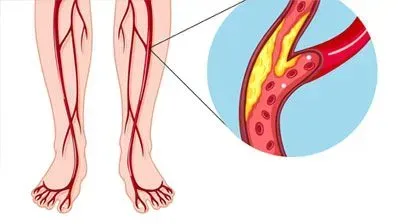
Diabetes is the leading cause of vasculopathies and neuropathies. It affects both the large and small blood vessels over time. Thus, most diabetes-related complications are due to worsening vascular health.
Diabetes is among the leading causes of heart disease, stroke, and peripheral artery disease. In addition, it is the leading cause of chronic kidney disease, retinopathy, and foot infections.
Diabetes and foot infection
Diabetes is the leading cause of foot infections. Data suggests that 25% of all those living with diabetes may expect to develop foot infection, sometimes in their lifetime. Nevertheless, there is a considerable difference in the severity of the infection between individuals. There are significant differences in the diabetes severity.
In diabetes, foot infection or diabetic foot wounds and ulcers occurs primarily due to changes in the blood supply. Peripheral vasculopathy causes significantly reduced blood flow to the feet. It means a reduced supply of nutrients, slow immune response, and thus considerable risk of developing the infection.
It is also worth understanding that diabetes foot infections may continue to progress if not managed adequately. Moreover, there are high chances of having multiple antibiotic-resistant infections. Studies suggest that about one-third of those infected have methicillin-resistant Staphylococcus aureus. Additionally, these wounds are infected by gram-negative bacilli and even anaerobes. Thus, diabetic food infections tend to be polymicrobial.
But not only that, due to low blood supply and changes in the nerve ending, foot infections also tend to behave very differently in those living with diabetes, and thus challenges in the treatment. For example, in diabetes, bacterial agents may form a biofilm and therefore not allow the entry of antiseptics into the wound.
Simply said, diabetes foot infection does not respond well to traditional treatments. It means a higher risk of spreading of the infection. Studies show that diabetes foot infection is the leading cause of non-traumatic foot amputation globally.
Diagnosis and treatment of diabetic foot infection
First and foremost, it is essential to understand that prevention is the best policy for diabetes. Thus, those living with severe diabetes should regularly inspect their feet. Moreover, due to neuropathy, many may not even feel the pain caused by minor trauma.
The treatment approach would depend on the severity of the condition:
Grade 1–almost no local or systemic signs of infection.
Grade 2 – local mild infection without the involvement of deeper tissues.
Grade 3 – moderate infection with severe abscess and infection affecting deeper tissues, causing osteomyelitis and severe systemic signs.
Grade 4 – local signs of severe infection with severe systemic symptoms.
When it comes to managing mild and moderate infections, doctors recommend strictly controlling the blood glucose level and antibiotic therapy. In the case of mild infection, oral antibiotic therapy may help. However, if the condition becomes severe, one would need systemic antibiotic therapy.
In more severe cases, doctors would need to carry out surgical treatment like debridement of the wound, which involves removing the dead tissues so that antibiotics can penetrate the living cells well.
Importance of diagnosing and treating peripheral artery disease in diabetes
Even the best treatment fails to prevent frequent foot infections in some individuals. Studies show that undiagnosed peripheral artery disease is the primary cause of foot infections progression in diabetes. It is the reason that leads to amputations. It means that doctors specializing in vascular diseases should be an essential part of the diabetic foot management team.
Those who have a diabetic foot infection, even a mild infection, should immediately seek help from a vascular surgeon. Studies estimate that peripheral arterial disease is present in 50-60% of all cases of diabetes foot infection.
Doctors may use many methods to assess the feet’ blood flow, like palpating pedal pulse. However, experts warn that it is not a reliable way of estimating the condition, and such physical signs are pretty unreliable, especially in the early stages of peripheral artery disease (PAD).
Generally, it is good to consult a specialized clinic in vascular disease management. In such clinics, doctors are well trained to diagnose and manage even minute vascular deficiencies. They would use various specialized equipment and procedures to diagnose the condition, from ultrasound to angiography.
If doctors find the presence of PAD, they may recommend treatment depending on the severity of the blockage. In less severe cases, they might recommend blood-thinning agents and other medications. However, more severe cases would need revascularization.
There are many ways of revascularization or improving blood flow to the feet, thus helping not only overcome foot infection in diabetes but also preventing amputation. Specialists may use methods like angioplasty, or more severe cases may need artery bypass graft (bypassing the blocked part of the blood vessel).
To conclude, managing PAD is an essential and yet one of the neglected ways of managing diabetic foot. Anyone living with diabetes and feet infection must understand that PAD is present in 50-60% of all diabetic foot infections. Thus, all people, even those with mild infections, should undergo examination at a specialized vascular disease management clinic. Not only that, depending on the severity of diabetes, one should preferably get checked by specialists at least once a year.
Importance of diagnosing and treating peripheral artery disease in diabetes
If you have diabetes, you know that even a tiny cut or sore on your foot can turn into a severe problem. That's because diabetes can damage the nerves and blood vessels in your feet, which can make it harder for your body to heal. If you have an open diabetic foot wound, properly caring for it is essential to prevent infection and other complications.
1. Keep the Wound Clean
Wash the wound gently with mild soap and water. Pat it dry with a clean towel. You may also use a saline solution to clean the wound. Avoid harsh chemicals or antiseptics, which can damage the tissue and delay healing.
2. Apply Antibiotic Ointment
Your doctor may prescribe an antibiotic ointment to help prevent infection. Apply a thin layer of ointment to the wound as directed.
3. Cover the Wound
Cover the wound with a clean, dry bandage. Change the bandage daily or more often if it gets dirty or wet.
4. Keep Pressure Off the Wound
Avoid putting pressure on the wound. This may mean wearing special shoes or using crutches. Your doctor can help you find the best way to keep pressure off your foot.
5. Monitor Your Blood Sugar
Keeping your blood sugar under control is essential for wound healing. Work with your doctor to manage your diabetes and keep your blood sugar levels within a healthy range.
6. See Your Doctor Regularly
It's essential to see your doctor regularly to monitor the wound and make sure it's healing correctly. If you notice any signs of infection, such as redness, swelling, or pus, immediately see your doctor.
Taking care of an open diabetic foot wound can be challenging, but it's essential to follow your doctor's instructions carefully. With proper care, your wound should heal without complications. If you have any questions or concerns, don't hesitate to contact our team at Advanced Vein & Vascular Management. We're here to help you keep your feet healthy!
Diabetic Foot Ulcers: A Silent Threat and How Advanced Treatments Can Help
Diabetes is a widespread health concern, and one of its lesser-known complications is the development of foot ulcers. These ulcers, often painless due to diabetic neuropathy (nerve damage), can escalate into severe infections and even amputations if left untreated. At Advanced Vein & Vascular Management, we understand the challenges faced by those with diabetic foot ulcers. Our team, led by Dr. Abedel Abushmaies, a renowned
diabetic foot ulcer doctor, provides advanced
diabetic foot ulcer treatment options that prioritize minimally invasive techniques and patient comfort.
Understanding the Severity of Diabetic Foot Ulcers
Diabetic foot ulcers form due to a combination of factors, primarily reduced blood circulation (peripheral artery disease) and nerve damage, both common in diabetic patients. These ulcers can become infected quickly; in severe cases, the infection can spread to the bone (osteomyelitis). This highlights the critical need for prompt and effective
diabetic foot ulcer treatment.
Imagine a patient, let's call him Mr. Smith, who noticed a small cut on his foot that wouldn't heal. Due to nerve damage, he experienced no pain, and the wound worsened over time. By the time he sought medical attention, the ulcer had become deeply infected. Unfortunately, this scenario is all too common.
Advanced Treatment Options for Diabetic Foot Ulcers
Traditional treatments for diabetic foot ulcers often involve wound debridement, dressings, and antibiotics. However, we go a step further at Advanced Vein & Vascular Management. Dr. Abushmaies, our expert
diabetic foot ulcer doctor, specializes in endovascular interventions, offering minimally invasive procedures that can significantly improve blood flow to the affected area, accelerating healing and reducing the risk of complications.
These procedures may include angioplasty, where a tiny balloon is used to widen narrowed arteries, or stenting, where a small mesh tube is inserted to keep the artery open. These techniques minimize discomfort and recovery time, allowing patients to regain mobility and quality of life sooner.
Prevention is Key: Practical Tips for Diabetic Foot Care
While advanced treatments are crucial, prevention remains the cornerstone of diabetic foot care. Here are some practical tips to keep in mind:
Taking Care of Your Feet When You Have Diabetes
- Inspect Your Feet Daily: Care carefully examine your feet for a few minutes each day. Look for any cuts, sores, blisters, redness, swelling, or changes in the toenails. A mirror can help you see the bottoms of your feet and those hard-to-reach areas. Early detection of any problems can prevent more severe complications down the road.
- Keep Your Feet Clean and Dry: Wash your feet daily with lukewarm water and mild soap. Avoid soaking your feet, as this can dry out the skin. After washing, dry your feet thoroughly, especially the areas between your toes. Excess moisture can create a breeding ground for bacteria and fungi.
- Moisturize Regularly: Dry skin can crack, leading to potential entry points for infection. Apply a good quality moisturizer to your feet daily, but avoid putting it between your toes. Look for moisturizers designed for feet, often containing ingredients that help prevent dryness and cracking.
- Choose the Right Footwear: Always wear comfortable, well-fitting shoes that provide adequate support and cushioning. Avoid shoes that are too tight or too loose or have seams that rub against your skin. It's also important to avoid going barefoot indoors and outdoors to protect your feet from injury.
- Schedule Regular Foot Exams: Even if you don't notice any problems with your feet, it's crucial to see a podiatrist or a
diabetic foot ulcer doctor regularly. They can perform a comprehensive foot exam, check for nerve damage and circulation problems, and guide proper foot care.
Remember, taking care of your feet is essential to managing diabetes. Following these simple tips can significantly reduce your risk of developing foot ulcers and other complications.
The Importance of Early Intervention
Early detection and intervention are crucial in managing diabetic foot ulcers. If you notice any non-healing sores or unusual changes in your feet, don't delay seeking professional help. Our Advanced Vein & Vascular Management team is committed to providing comprehensive
diabetic foot ulcer treatment, from minimally invasive procedures to guidance on proper foot care.
Remember, diabetic foot ulcers are a severe complication, but with proper care and advanced treatment options, you can significantly reduce the risk of severe consequences.
Contact Advanced Vein & Vascular Management today to schedule a consultation and learn more about how we can help you manage diabetic foot ulcers and maintain healthy feet.
References
- National Diabetes Statistics Report | Diabetes | CDC. Published January 20, 2022. Accessed April 3, 2022. https://www.cdc.gov/diabetes/data/statistics-report/index.html
- Uçkay I, Aragón-Sánchez J, Lew D, Lipsky BA. Diabetic foot infections: what have we learned in the last 30 years? International Journal of Infectious Diseases. 2015;40:81-91. doi:10.1016/j.ijid.2015.09.023
- Boulton AJM, Armstrong DG, Kirsner RS, et al. Diagnosis and Management of Diabetic Foot Complications. American Diabetes Association; 2018. Accessed April 3, 2022. http://www.ncbi.nlm.nih.gov/books/NBK538977/
Diabetic Foot Infection FAQ
Why are diabetic foot ulcers so dangerous?
Diabetic foot ulcers are a severe health risk because they involve several factors that make them difficult to heal. Poor blood flow to the feet slows down the body's natural ability to repair itself, making these ulcers prone to infection. Also, many people with diabetes experience nerve damage in their feet, which can cause numbness. This means they might not feel a cut or sore developing, allowing it to worsen without their knowledge. If left untreated, these infections can become severe and even spread to the bone, potentially leading to amputation.
How can I prevent diabetic foot ulcers?
Comfort is key when it comes to preventing diabetic foot ulcers. Always wear comfortable shoes that fit well to protect your feet from injury. This will help you feel at ease and reduce the risk of developing ulcers. In addition to this, it's important to check your feet every day for any signs of trouble, like cuts, blisters, or redness. Keeping your feet clean and dry is also important to avoid infection. Remember to moisturize regularly to prevent cracks in the skin. And remember, seeing a foot specialist regularly is also a good idea, even if you think your feet are fine. They can help you catch any problems early on and keep your feet healthy.
What are the latest treatment options for diabetic foot ulcers?
At Advanced Vein & Vascular Management, we go beyond primary wound care for diabetic foot ulcers. Dr. Abushmaies, a skilled specialist in minimally invasive procedures, uses techniques like angioplasty and stenting to improve blood flow in the affected area. This helps ulcers heal faster and lowers the chance of complications. These procedures are much less invasive than traditional surgery, meaning less discomfort and a quicker recovery for our patients.